Deworming Schedules for Puppies & Kittens
Deworming Puppies and Kittens: A Simple Schedule for New Pet Owners
Bringing home a new puppy or kitten is a whirlwind of tiny paws and endless snuggles. While toys, food, and snuggles come first, internal parasites may not be on your radar. Worms are common in young pets and can cause real issues, so it’s important to protect them early. The good news: with the right plan, prevention and treatment are simple.
We know all the puppy and kitten “must-dos” can feel like a lot, but parasite protection is one of the most important steps in your pet’s early health. At Harbor Pines Veterinary Center in Harbor City, CA, we include deworming in our comprehensive wellness care and preventive services. As an AAHA-certified practice, we’ll set a clear, easy schedule and answer your questions along the way. Have a new pet? Request an appointment with our caring team.
Puppy and Kitten Deworming: Why It Matters From Day One
Most puppies and kittens are exposed to worms before coming home, even if they look healthy. Parasites steal nutrients, irritate the gut, and in heavy loads can cause blood loss or blockages. Early deworming supports steady growth and comfort.
Many pups and kittens acquire intestinal parasites from their mothers or environments, and young immune systems can’t control parasites well, so burdens rise quickly. Some worms are zoonotic parasites and can infect people, which adds another reason to start protection right away.
Deworming is part of a bigger plan alongside vaccines, nutrition, and growth checks in our wellness care and preventive services.
What Worms Do Puppies and Kittens Get?
Roundworms and Hookworms: The Frequent Offenders
Roundworms are often passed before birth or through milk. You might see a potbelly, vomiting, diarrhea, or a dull coat. Hookworms attach to the intestinal lining and feed on blood, which can lead to pale gums and weakness in small pets. Transmission can occur during pregnancy, nursing, or from contaminated soil. You may even notice spaghetti-like strands in stool or vomit. Because some species are zoonotic parasites, preventing and promptly treating infections protects the entire family.
Whipworms and Tapeworms: Less Obvious, Still Important
Whipworms live in the large intestine and can cause intermittent diarrhea and weight loss, especially in dogs. Eggs can persist in soil for years, making cleanup and testing important.
Tapeworms are linked to fleas. Pets get them by swallowing an infected flea while grooming, and owners often notice rice-like segments near the tail. Preventing tapeworms starts with solid flea control and understanding flea life cycles. In short, environmental persistence matters for whipworms, and reliable flea prevention is key to tapeworm control.
Protozoal Parasites: Coccidia and Giardia
Single-celled parasites can cause diarrhea and dehydration, especially in crowded settings like shelters. Coccidia and giardia spread through contaminated water, soil, or feces. Symptoms range from soft stool to severe diarrhea, and good hygiene plus clean water sources reduce risk significantly.
To confirm what’s present and tailor treatment, we use fecal testing through our laboratory services for fast, targeted care.
What Is the Recommended Deworming Schedule for Puppies and Kittens?
The Early-Week Protocol That Sets the Foundation
A simple rule gets most young pets on track: start at two weeks of age, then repeat every two weeks until 16 weeks or the fecal test comes back negative. This cadence targets worms at multiple life stages and aligns with common parasite life cycles and public health guidance. We integrate this into new-pet visits and adjust as needed so it lines up with vaccines and growth checks. Ready to get started? Schedule wellness care and we’ll map out the plan.
Deworming at Six Months and One Year
A check at six months and again at one year helps catch new infections as your pet explores parks and beaches. These visits are perfect for fecal testing and reviewing your prevention plan. Fecal testing verifies prevention is working and these milestones transition your pet into an adult plan. Our health exams include a full assessment and a customized parasite roadmap.
Moving From Deworming to Long-Term Prevention
Why Year-Round Preventive Medications Matter
After the initial series, monthly preventives help protect against multiple intestinal worms and often include heartworm prevention. In Southern California’s mild climate, parasites stay active most of the year, so year-round parasite prevention is a smart move.
- One monthly routine is easier to remember and covers more ground.
- Mild winters around Harbor City mean ongoing exposure.
Routine Fecal Testing Keeps You Ahead of Problems
Microscopic stool exams detect eggs too small to see. Puppies and kittens typically need two to four fecal tests in the first year, then twice yearly for adults living active lifestyles. Most boarding facilities and daycares require negative tests. Because pets can carry parasites without symptoms, testing offers peace of mind and lets us adjust prevention plans based on real results. If it’s been a while, book an appointment today.
How Lifestyle Shapes Your Pet’s Deworming Plan
Every pet’s routine is different, and parasite control should reflect that. Indoor cats may have lower risk than beach-loving dogs, but exposure can still happen through shoes, houseplants, or fleas. Tell us about daily habits like outdoor time on soil or grass, any hunting behavior, time spent in parks or daycares, contact with wildlife or strays, and travel to different regions. We translate those details into a right-sized plan during wellness visits. If clinic visits are difficult, our mobile services bring care to you so your pet stays on schedule.
Protecting Your Family From Parasites That Can Spread to People
Some parasites can infect people, especially kids playing where pets go. Simple habits cut the risk significantly. Pick up stool promptly and dispose of it in sealed bags, wash hands after handling pets or working in soil or sand, cover sandboxes and avoid barefoot play in areas where pets relieve themselves, and keep pets on preventives while following testing schedules. Paired with your veterinary plan, these routines keep everyone safer. Have questions about family hygiene around pets? Our team can help.
What Happens During a Deworming Visit?
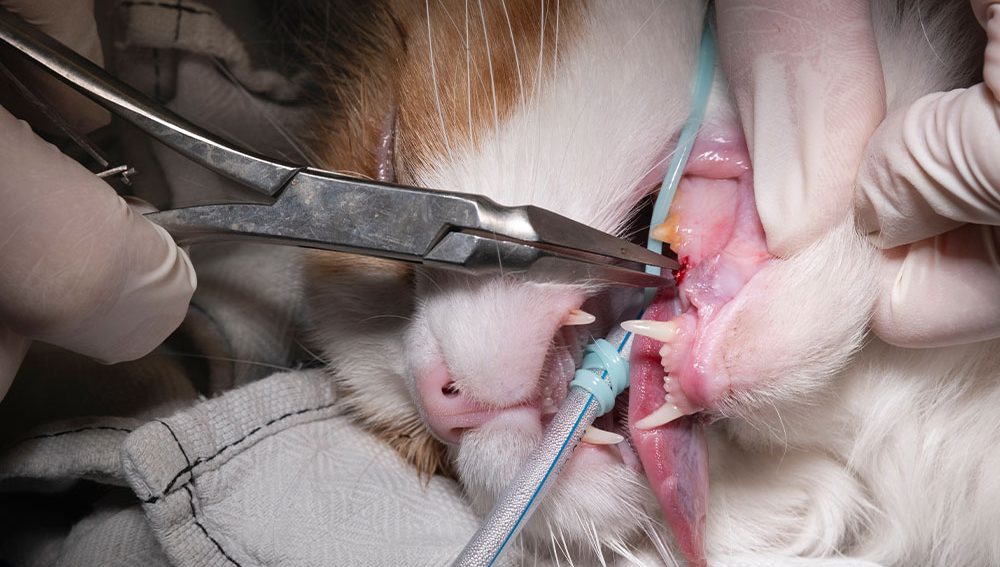
Appointments focus on accurate dosing and comfort. We start with a physical exam and current weight to tailor medication. Depending on the product, treatment is given by mouth, injected, or applied to the skin. Most dewormers are safe and well-tolerated, though mild digestive upset may occur briefly. Bringing a fresh stool sample lets us confirm what’s present and ensure the chosen medication is the best fit. If anything seems off after treatment, contact us. Ready to bundle vaccines and parasite care? Request an appointment and we’ll guide you every step.
A Practical Deworming Timeline You Can Follow
Keep this quick-reference schedule handy:
- As a puppy or kitten: Deworm every two weeks until the last set of vaccines and/or fecal test is negative.
- Six months: Wellness exam, fecal test, deworm if needed.
- One year: Annual exam, fecal test, vaccines if indicated.
- Ongoing: Begin monthly preventives for intestinal worms, fleas, and heartworm as early as possible.
Tie this to vaccine visits for an easy routine. Our vaccination services align with parasite protocols for comprehensive protection.

Local Notes for Harbor City Pet Parents
Our coastal climate keeps outdoor adventures going most of the year, and that keeps parasites active. Sand, soil, and shared green spaces can harbor eggs, and warm spells fuel flea activity. If your family enjoys hikes and beach time, stick with monthly preventives and regular fecal tests. If transportation or schedules are tough, we can come to you with the same AAHA-level care. Explore our mobile services to stay on time.
FAQs: Quick Answers for New Pet Parents
Do indoor-only pets need parasite prevention?
Yes. Exposure can happen through shoes, fleas, potting soil, or new pets, so prevention and periodic fecal tests are still important.
How will I know if my pet has worms?
Signs can include soft stool, vomiting, a potbelly, or rice-like segments near the tail. Many pets show no signs, which is why routine fecal testing helps.
Are over-the-counter dewormers enough?
Not always. Different parasites need different medications and dosing. A fecal test helps target the right treatment and avoid missed infections.
Can people catch worms from pets?
Some parasites can infect humans. Consistent preventives, picking up stool promptly, and handwashing reduce risk significantly.
Growing Up Healthy: Your Guide to Lifelong Parasite Protection
Thoughtful deworming in the early weeks, monthly prevention, and routine fecal testing give your puppy or kitten their best start while protecting your family. Our AAHA-certified team pairs quick diagnostics with compassionate care to design a plan that fits your home and routine. We coordinate deworming with vaccines and wellness visits for seamless protection.
If you’re ready for a personalized schedule or have questions about symptoms, explore our services and contact us to schedule your pet’s wellness visit. We’re here to help, guide, and be your partner in your pet’s care so parasite prevention stays simple and stress-free.